Ben Valsler
我们遇到的一个问题和平面nt coronavirus outbreak has been the volume of poorly communicated, unclear or simply misleading information out there, especially on social media. This week’s compound, ibuprofen, has been at the heart of some of that, with stories circulating on whatsapp groups in particular claiming that it would make the symptoms of Covid-19 worse. Many of these claims are false, bearing the names of made-up doctors or attributed to institutions that have made no such statements.
The truth is not entirely clear – no studies have been done on ibuprofen and Covid-19, so there’s no results to report – but there are some concerns, so the NHS guidance in the UK is now to takeparacetamolto lower your fever, rather than ibuprofen. I’m sure people share these posts to be helpful, but as always, consult your doctor – not your social feeds – before changing your medication.
Brian Clegg put together this podcast before the pandemic, so that aspect is not covered here, but it does fill a shocking gap in our podcast catalogue, one of the most widely used over-the-counter painkillers of recent decades.
Brian Clegg
Read any old novel and someone with a headache is liable to reach for an aspirin, but modern over-the-counter painkilling is dominated by two more recently discovered compounds – paracetamol and ibuprofen. Of these, ibuprofen, like aspirin, has the advantages of being an anti-inflammatory, so is particularly good for muscle pain, but has less impact on the stomach than its older cousin. It also presents a lower overdose risk than paracetamol.
Often sold under brand names such as Nurofen, Brufen and Advil, ibuprofen – a tongue-twisting contraction of isobutyl propanoic phenolic acid – is a relatively simple aromatic acid with a single benzene ring at its centre. Unusually for such a widely used drug, it was not developed by a major pharmaceutical company but by the British pharmacy chain Boots, from the simple organic fatty acid propanoic acid – effectively acetic acid with an added methyl group – a compound that had been known since the 1840s.
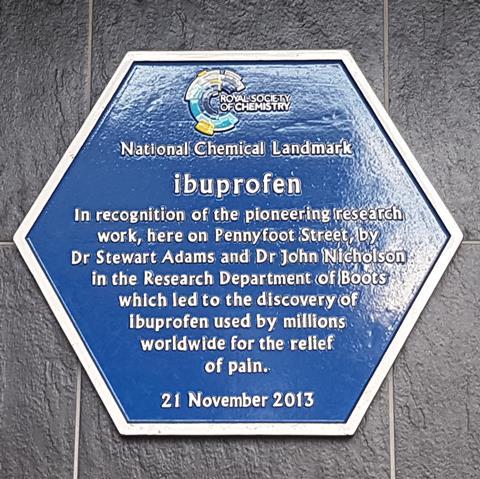
Ibuprofen was developed in 1961 at the Boots laboratory in Nottingham by a team led by Stewart Adams and John Nicholson. The primary focus was a drug for rheumatoid arthritis, which was treated at the time with steroids, bringing with them significant side effects. The aim was to develop a non-steroidal anti-inflammatory drug that did not have the same risk of gastrointestinal bleeding that accompanied the high doses of aspirin that were the only such option at the time. After spending nearly 10 years testing around 600 compounds, the team homed in on what would become ibuprofen. The new development proved to be a significantly stronger general painkiller than paracetamol, which had by then been on the market for a few years.
Adams tested its effectiveness when he was due to make a speech, but was suffering from his previous night’s drinking. ‘I was first up to speak and I had a bit of a headache after a night out with friends. So I took a 600mg dose, just to be sure, and I found it was very effective.’ Ibuprofen was licenced in the UK in 1969 and the US in 1974, moving to over-the-counter status a little over ten years later.
The drug works by cutting down the hormones that cause pain and swelling – in effect it is calming down the body’s defences. Specifically, it acts on a series of enzymes known as cyclooxygenase, reducing the body’s ability to produce prostaglandins. These are special molecules used by the body to carry signals to cells to deal with immune system responses.

Like all medications, ibuprofen has potential side-effects and carries some risks. There was concern in 2017 when the European Society of Cardiology announced that ‘painkillers considered harmless by the general public are associated with increased risk of cardiac arrest.’ Specifically, a large study from Denmark of patients who had an out-of-hospital heart attack between 2001 and 2010 (a total of 28,947 individuals) appeared to show that use of ibuprofen increased the risk of cardiac arrest by 31 percent. This led to headlines such as the Guardian’s ‘Calls for ibuprofen sale restrictions after study finds cardiac arrest risk.’ But is this response justified?
The study only considered prescribed doses of ibuprofen, which are often much higher and taken for significantly longer than the over-the-counter doses most users encounter. It wasn’t clear from the study that there was a causal link between taking the drug and the heart attacks. Most importantly, the study made the serious mistake of only providingrelativerisk, which can be extremely misleading. In a blog post for the Winton Centre for Risk and Evidence Communication at the University of Cambridge, Michael Blastland estimated if the effect really was causal, the impact of taking ibuprofen would be one extra cardiac arrest in every 32,000 people over the 30 day period before the event – which sounds very different from a 31 per cent increase.
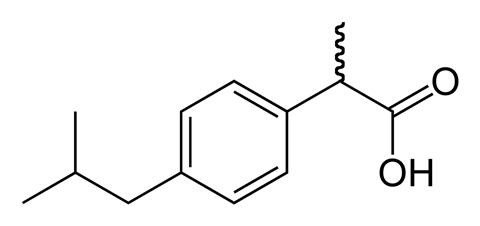
On a positive note, it has also been shown that there is a possibility that ibuprofen could be used to treat prostate cancer. This potential treatment demonstrates the action of an oddity of ibuprofen’s chirality. This is its handedness – like a pair of gloves, the ibuprofen molecule comes as two similar looking but mirror-image variants. An enzyme known as AMACR has been shown to catalyse a change in handedness of a molecule apparently related to tumour cell growth. But AMACR also converts one form of ibuprofen into the other, and it appears that while it is doing so, AMACR is prevented from promoting the growth of cancer cells. These early findings from 2011 will not necessarily result in a treatment, but demonstrate the significance of the ibuprofen molecule’s chirality.
Ibuprofen has gone on to join the World Health Organisation’s ‘List of Essential Medicines’, regarded as the core medical toolkit. More than 20,000 tonnes of ibuprofen help millions suffering from pain, inflammation and fevers each year. Not bad for a medication that had humble beginnings in the research lab of a chain of high street chemists.
Ben Valsler
That was Brian Clegg with ibuprofen.
Next week, another established drug returns to the headlines, as anti-malarial chloroquine is being touted as a potential treatment for Covid-19. I have some personal experience with chloroquine, having taken it to avoid malaria in Bolivia and Indonesia, so I’ll round up its history and potential role in our current pandemic next time. Until then, get in touch with any comments or suggestions of compounds to cover – emailchemistryworld@rsc.orgortweet @chemistryworld. And you can find the entire back catalogue of Chemistry in its element podcasts atchemistryworld.com/podcasts– if you see any other obvious ones, like ibuprofen, that we’ve missed, do let us know and we’ll be sure to catch up. I’m Ben Valsler, thanks for joining me.
Additional information
Theme:OpifexbyIsaac Joel, via Soundstripe
Additional music:星期天byMarie, via Soundstripe








No comments yet